Living with unexplained changes in your body can be frustrating and worrisome, especially when they disrupt your daily routine and leave you feeling off-balance. These subtle shifts might seem minor at first, but they can build up, affecting your energy, mood, and overall well-being in ways that make everyday tasks feel exhausting. Fortunately, recognizing these patterns early can empower you to take proactive steps toward better health. But here’s the intriguing part: one lesser-known sign could be hiding in plain sight on your skin—stick around to uncover it at the end.
Understanding Diabetes and Why Early Awareness Matters
Diabetes is a condition where your body struggles to manage blood sugar levels effectively, often due to issues with insulin production or use. According to the Centers for Disease Control and Prevention (CDC), millions of people live with it unknowingly, which highlights the importance of paying attention to your body’s signals.
But that’s not all—early detection through lifestyle adjustments and professional guidance can make a significant difference in how you feel day to day.
Research from the American Diabetes Association shows that prediabetes, a precursor stage, affects about 1 in 3 adults in the U.S., yet many overlook the initial indicators.
This awareness isn’t about fear; it’s about equipping yourself with knowledge to maintain your vitality.
The 10 Early Signs to Be Mindful Of
Let’s break this down into clear, manageable sections. We’ll explore each sign, what it might feel like, and simple ways to monitor it.
1. Increased Thirst and Frequent Urination
One common early indicator is feeling unusually thirsty, even after drinking plenty of fluids. This happens because high blood sugar pulls water from your tissues, leaving you dehydrated.
You might find yourself visiting the bathroom more often, especially at night, which can interrupt sleep and lead to fatigue.
To track this, keep a simple journal of your fluid intake and bathroom trips for a week.
Studies from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) suggest this duo of symptoms is often the first noticeable change.
But wait, there’s more to consider—let’s move to the next one.

2. Unexplained Weight Loss
If you’re shedding pounds without changing your diet or exercise routine, it could be a signal. Your body might be breaking down muscle and fat for energy when it can’t use glucose properly.
This can feel confusing, as you might expect weight gain instead.
A practical tip: Weigh yourself weekly under the same conditions and note any patterns.
Research published in the Journal of the American Medical Association indicates this occurs in about 40% of people before a formal diagnosis.
Sustainability is key here—small observations add up.
3. Persistent Hunger
Even after eating a full meal, you might still feel ravenous. This polyphagia, as it’s known, stems from cells not getting the energy they need from food.
It can lead to overeating or constant snacking, which might exacerbate the cycle.
Try this: Opt for balanced meals with protein, fiber, and healthy fats to see if it stabilizes your hunger.
The Mayo Clinic reports this as a classic early marker in their patient education resources.
And speaking of energy, the next sign ties right in.
4. Fatigue and Low Energy
Feeling tired all the time, despite getting enough rest? When sugar builds up in your blood instead of fueling your cells, exhaustion sets in.
This can make workouts or even simple chores feel overwhelming.
Action step: Incorporate short walks or stretches into your day and monitor how your energy responds.
According to Harvard Health Publishing, chronic fatigue is linked to metabolic imbalances in numerous studies.
But here’s something interesting: it often pairs with vision changes.
5. Blurred Vision
Temporary blurriness or difficulty focusing might occur as high blood sugar causes lens swelling in your eyes.
It usually resolves with blood sugar stabilization, but it’s worth noting.
Simple advice: Schedule regular eye check-ups and mention any fluctuations.
The American Optometric Association emphasizes early eye exams for at-risk individuals.
Now, let’s shift to physical sensations.
6. Slow-Healing Sores or Cuts
If minor injuries take longer than usual to heal, it could indicate impaired circulation or immune function related to blood sugar levels.
This might show as persistent bruises or infections.
Tip: Keep wounds clean and covered, and track healing time.
WebMD cites this as a key observation in their diabetes overviews, backed by clinical data.
The truth is, this can extend to frequent infections.

7. Frequent Infections
Yeast infections, urinary tract issues, or skin infections might recur more often due to sugar-rich environments fostering bacteria and fungi.
Women may notice this in particular areas.
Practical step: Maintain good hygiene and stay hydrated to support your body’s defenses.
Research from the Journal of Clinical Investigation supports this connection.
And don’t overlook tingling sensations.
8. Numbness or Tingling in Hands and Feet
Known as neuropathy, this pins-and-needles feeling results from nerve damage over time.
It often starts subtly in extremities.
To address: Wear comfortable shoes and check your feet daily for changes.
The National Institutes of Health (NIH) documents this in their neuropathy fact sheets.
But that’s not the end—skin changes are next.
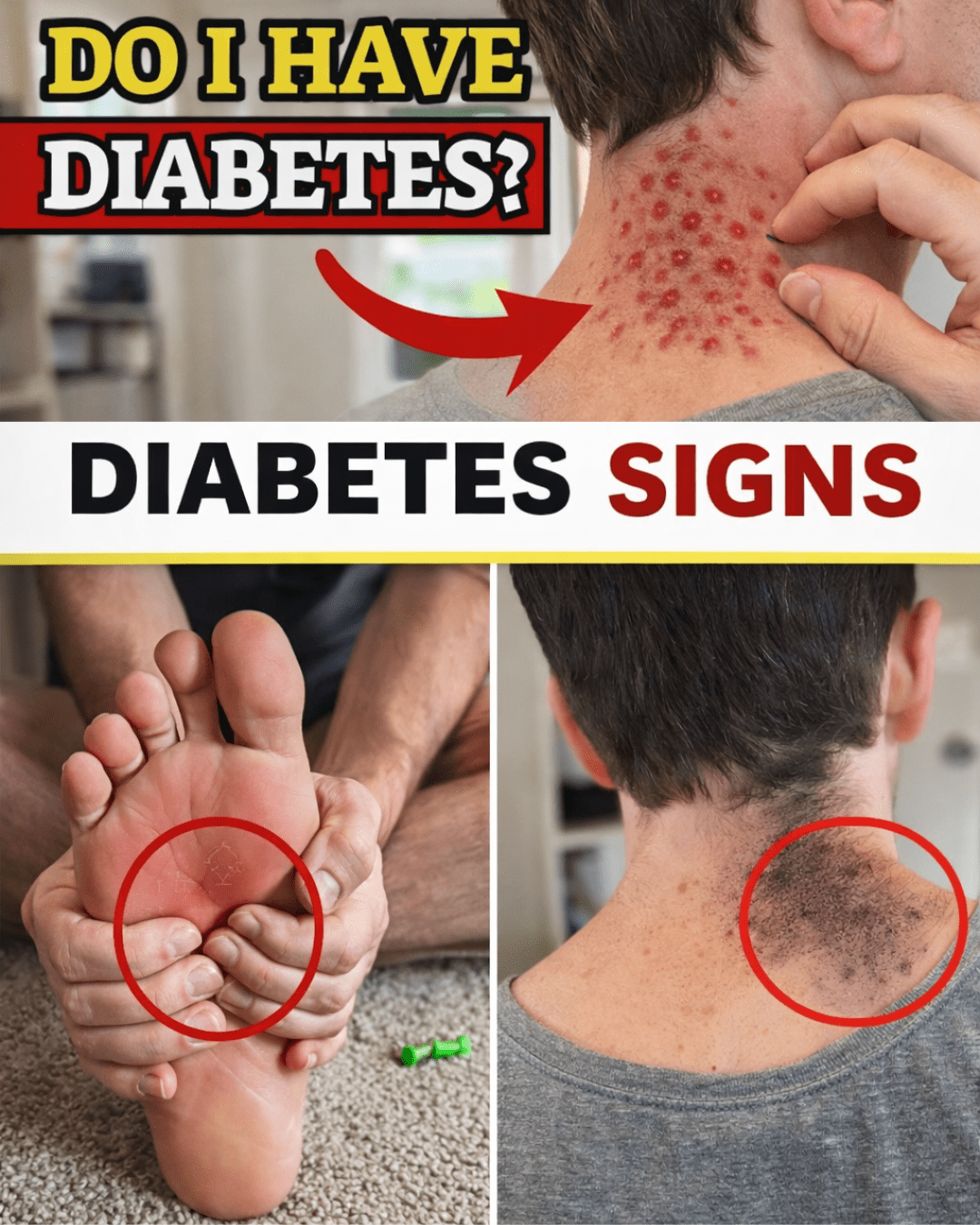
9. Itchy Skin or Rashes
Dry, itchy skin or unexplained rashes can appear, sometimes due to poor circulation or yeast overgrowth.
You might notice this on legs or other areas.
Suggestion: Use moisturizers without added fragrances and observe improvements.
Dermatology studies in the British Journal of Dermatology link this to metabolic factors.
Finally, the one we hinted at earlier.
10. Darkened Skin Patches (Acanthosis Nigricans)
This velvety, dark discoloration often appears on the neck, armpits, or groin, signaling insulin resistance.
It’s more common in certain ethnic groups and overweight individuals.
Quick tip: Gently cleanse the area and consult if it persists.
The CDC highlights this as an early visual cue in their awareness campaigns.
How to Monitor These Signs at Home
Staying on top of these doesn’t require fancy tools. Here’s a straightforward guide:
- Daily Check-Ins: Spend 5 minutes noting thirst, energy, or skin changes in a notebook or app.
- Blood Sugar Tracking: Use over-the-counter glucose monitors if you suspect patterns—follow instructions carefully.
- Lifestyle Tweaks: Incorporate balanced meals, like veggies with lean proteins, and aim for 30 minutes of movement daily.
These steps can help you gather information before seeking professional input.
Comparing Type 1 and Type 2 Diabetes Signs
To provide clarity, here’s a simple table:
| Aspect | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Onset | Sudden, often in youth | Gradual, usually in adults |
| Common Signs | Thirst, urination, weight loss | Fatigue, blurred vision, slow healing |
| Risk Factors | Autoimmune, genetics | Lifestyle, obesity, age |
| Management Focus | Insulin therapy | Diet, exercise, medications |
This overview, drawn from ADA guidelines, helps differentiate without overwhelming.
When to Seek Professional Advice
If multiple signs align, it’s wise to discuss with a healthcare provider. They can offer tailored insights based on tests.
Remember, self-monitoring is empowering, but expert guidance ensures accuracy.
Studies show early intervention supports better long-term outcomes.

Conclusion
Being aware of these 10 early signs—increased thirst, weight loss, hunger, fatigue, blurred vision, slow healing, infections, numbness, itchy skin, and darkened patches—can help you stay proactive about your health. Small daily habits like tracking symptoms and balanced eating go a long way. By recognizing these signals, you’re taking a positive step toward well-being.
FAQ
What lifestyle changes can support blood sugar balance? Focus on whole foods, regular activity, and stress management techniques like walking or meditation, as suggested by health organizations.
How often should I check for these signs? A weekly self-assessment is a good start, but consult a professional if changes persist for more than a few weeks.
Are these signs always related to diabetes? Not necessarily—they can stem from other causes, so professional evaluation is key for context.
Disclaimer: This article is for informational purposes only and not a substitute for professional medical advice. Always consult a healthcare provider for personalized guidance.
(Word count: 1,248)