Many people start metformin to help manage their blood sugar levels when living with type 2 diabetes or prediabetes. This medication has been a trusted option for decades because it supports better glucose control without causing weight gain in most cases. Yet, while doctors often highlight its benefits during short visits, some longer-term or less frequent effects might not come up as often. These can sometimes catch people by surprise, leading to questions about energy dips, digestive changes, or other subtle shifts.
It’s common to wonder if certain feelings are connected to the medication or just part of daily life with diabetes. Research shows that awareness of these possibilities can make a big difference in how people feel day to day. But here’s the encouraging part: many of these can be monitored or managed with simple steps. Keep reading to explore what studies and reliable sources reveal—and discover practical ways to stay ahead.
Why Some Metformin Effects Might Not Be Discussed Right Away
Metformin works by helping the body use insulin more effectively and reducing glucose production in the liver. Guidelines from organizations like the American Diabetes Association recommend it as a first-choice option for many. That’s because large studies, including the Diabetes Prevention Program, have shown it helps with blood sugar management over time.
However, busy appointments focus on getting started safely. Less common or gradual effects, which research links to longer use, might not always get full attention upfront. The good news? Many people tolerate it well, and awareness allows for better conversations with healthcare providers.
Here’s a quick overview of how common some effects are, based on studies:
- Very common (up to 30% of users): Digestive discomfort like nausea or loose stools, often improving with time.
- Common with longer use: Changes in nutrient absorption.
- Rare: More serious concerns that need prompt attention.
But that’s just the start. Let’s dive deeper.
#1 The Rare Concern of Lactic Acidosis: What to Watch For
Lactic acidosis happens when lactate builds up in the blood, making it more acidic. While very uncommon with metformin—studies estimate fewer than 10 cases per 100,000 patient-years—it’s taken seriously because it can be significant if it occurs.
Research indicates higher chances in situations like reduced kidney function or dehydration. Symptoms might include unusual tiredness, muscle aches, or breathing changes.
Quick tip: Stay hydrated and discuss kidney checks with your doctor regularly. If anything feels off suddenly, reach out right away.
#2 That Unusual Taste in Your Mouth
Some people notice a metallic or odd taste, especially early on. This dysgeusia comes from how metformin interacts in the body and often fades as you adjust.
Studies note it affects appetite for a few, but simple adjustments like eating with meals can help.
Have you noticed any taste changes? Trying sugar-free gum or timing doses differently might make a difference.

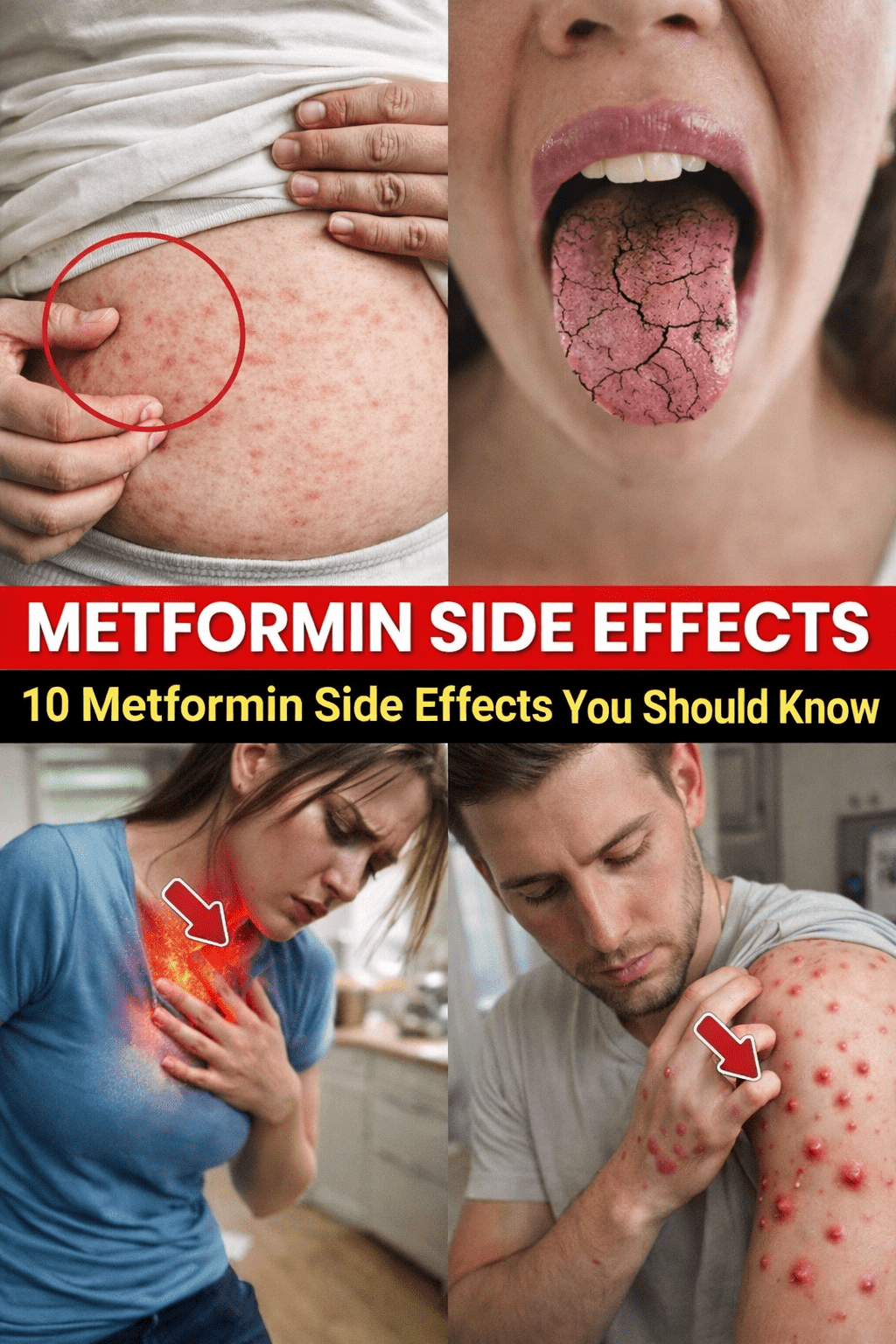
#3 Skin Changes Worth Noting
Though not frequent, reports include rashes, itching, or hives in some users. Reliable sources like Mayo Clinic list these as possible reactions.
Most are mild and resolve, but monitoring new skin shifts is wise.
Actionable step: Track any changes in a journal and share with your provider if they persist.
#4 How Metformin Can Affect Vitamin B12 Levels Over Time
Long-term use may reduce B12 absorption in the gut. Studies, including the Diabetes Prevention Program Outcomes Study, show this risk increases after years of use, potentially leading to lower levels.
Low B12 might contribute to fatigue or tingling sensations.
Research suggests annual checks for those on it long-term, especially over age 65 or higher doses.
Practical ways to support B12:
- Include foods like eggs, fish, or fortified cereals.
- Ask about testing—simple blood work can guide if supplements are needed.
- Many find levels stabilize with monitoring.
This is one area where early awareness pays off.
#5 Digestive Discomfort: The Most Reported Issue
Up to 30% experience nausea, bloating, or diarrhea, per reviews in journals like Diabetes, Obesity and Metabolism. These often peak early and ease.
But wait—there’s more that helps many.
Tips to ease GI effects:
- Start low and increase slowly.
- Take with food.
- Consider extended-release versions—studies show fewer issues.
- Stay hydrated and eat smaller meals.
Most find it improves within weeks.
#6 Changes in Weight: What Studies Show
Some notice modest weight reduction, around 2-3 kg in trials. This can support diabetes management but feels unexpected for others.
Monitor patterns and discuss nutrition to keep it balanced.
#7 Low Blood Sugar Episodes
Rare alone, but possible with fasting or combined meds. Signs include shakiness or confusion.
Carry quick carbs and know your patterns.
#8 Reports of Hair Thinning
Occasional case reports link it, possibly via B12 changes, but not common in large studies.
If noticed, check nutrients and rule out other factors.

#9 Fatigue and Anemia Connections
Low B12 or other shifts might play a role in tiredness. Blood tests help clarify.
#10 Rare Links to Pancreatitis
Case reports exist, but uncommon. Severe belly pain warrants immediate check.
Overview of Key Insights from Research
| Insight | How Often Noted | Common Signs | Helpful Steps |
|---|---|---|---|
| Lactic Acidosis | Rare | Muscle pain, breathing changes | Kidney monitoring, hydration |
| Unusual Taste | Common early | Metallic flavor | Dose with meals |
| Skin Changes | Uncommon | Rash, itch | Track and report |
| B12 Impact | Longer-term | Fatigue, tingling | Annual tests, foods/supplements |
| Digestive Issues | Very common | Nausea, diarrhea | Extended-release, slow start |
| Weight Shifts | Common | Gradual loss | Balanced eating |
| Low Blood Sugar | Rare alone | Shakiness | Quick carbs handy |
| Hair Changes | Rare reports | Thinning | Nutrient checks |
| Anemia Risk | Uncommon | Tiredness | Blood work |
| Pancreatitis | Rare | Severe pain | Urgent care if needed |
Simple Monitoring Timeline to Stay Proactive
- First month: Note any digestive adjustments.
- Every 3-6 months: Discuss how you’re feeling.
- Annually: Consider B12 and kidney checks, per many guidelines.
- Ongoing: Journal symptoms for patterns.
These habits empower better discussions.
Frequently Asked Questions
How common are digestive issues with metformin?
Studies show up to 30% notice them, mostly mild and temporary. Extended-release often helps.
Should I worry about vitamin B12?
Longer use raises chances of lower levels. Research supports checking yearly if on it for years—talk to your doctor.
When should I contact my healthcare provider?
For sudden severe symptoms, new rashes, extreme fatigue, or breathing changes—always reach out promptly.
Final Thoughts
Staying informed about these insights helps many feel more in control while managing diabetes. Simple monitoring and open talks with providers make a real difference. You’re already taking positive steps by learning more.
This article is for informational purposes only and is not medical advice. Always consult your healthcare provider about your medication, symptoms, or changes to your routine. They know your full history best.