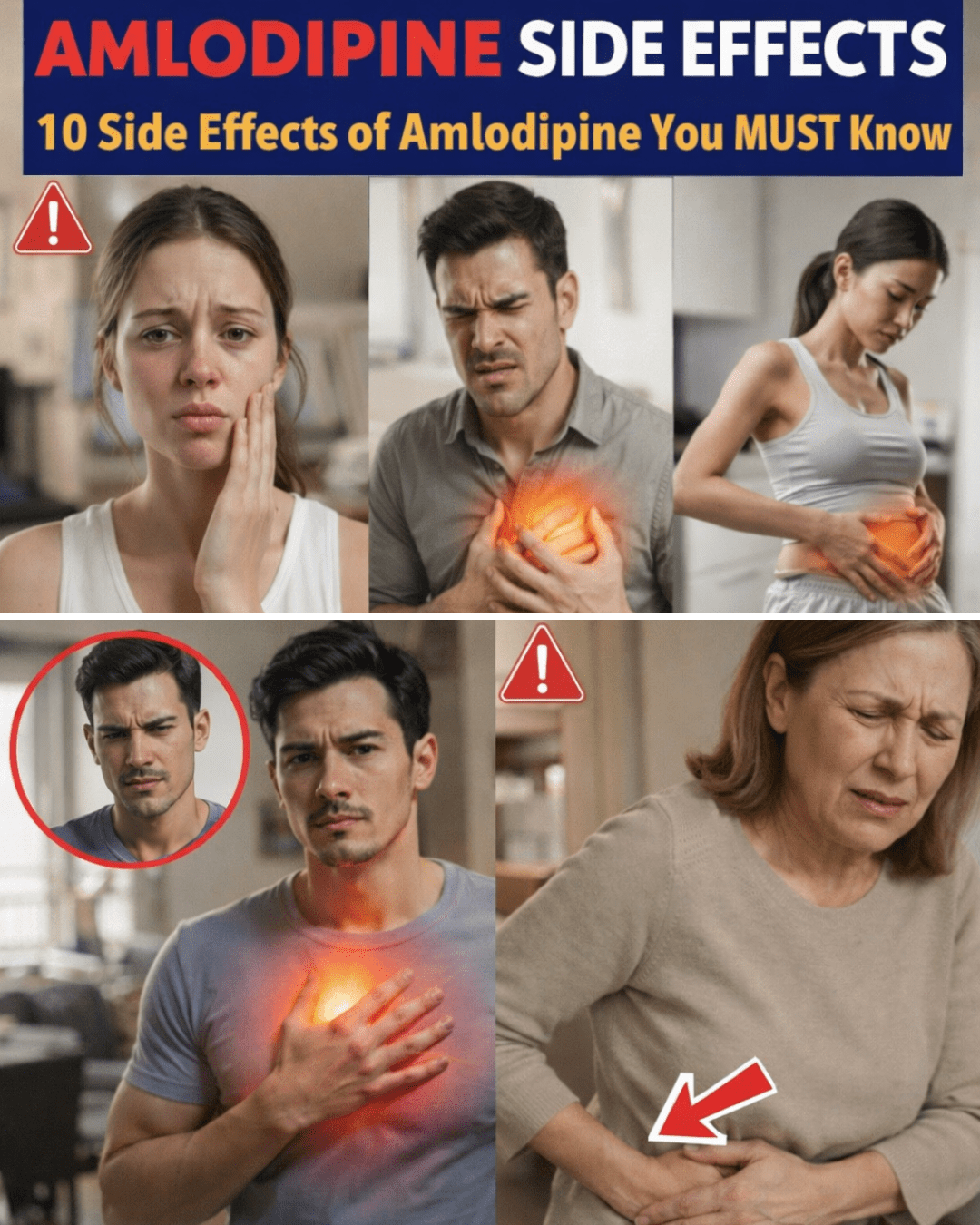
You take your daily amlodipine to help manage high blood pressure, but then you notice your ankles look a bit swollen at the end of the day, or you feel a sudden warmth in your face that catches you off guard. These moments can leave you wondering if something’s wrong or if it’s just part of taking the medication. Many people experience these sensations, and while they’re often mild and temporary, they can still feel unsettling and disrupt your routine.
The good news is that understanding why these effects happen can bring clarity and confidence. In this guide, we’ll explore the most common side effects of amlodipine, what causes them, and simple lifestyle habits that may help you feel more comfortable while staying on track with your treatment.
Why Do Side Effects Happen with Amlodipine?
Amlodipine is a calcium channel blocker that relaxes and widens blood vessels, making it easier for blood to flow and helping lower blood pressure. This same action can sometimes lead to shifts in fluid distribution or changes in blood flow that result in noticeable sensations. Research shows these effects are usually dose-related and more common when starting or increasing the dose, but they often improve as your body adjusts.
But here’s the key: not everyone experiences side effects, and when they do occur, they’re typically mild. The following sections break down the most commonly reported ones, based on reliable sources like clinical studies and patient reports.
Common Side Effects and What They Might Feel Like
Studies and patient experiences highlight several effects that tend to appear more frequently. Here’s a closer look at the top ones.
1. Swelling in the Ankles or Feet (Edema)
This is one of the most reported effects, often showing up later in the day or after standing for long periods. Fluid can pool in the lower extremities because widened vessels allow some leakage into surrounding tissues.
2. Flushing or Warmth in the Face
You might feel a sudden warmth or redness in your cheeks, similar to a hot flash. This happens as blood vessels dilate, increasing flow near the skin’s surface.
3. Dizziness or Lightheadedness
Standing up quickly can cause a brief dizzy spell as blood pressure adjusts. This is more common early on or if you’re dehydrated.
4. Fatigue or Feeling Tired
Some people describe a general sense of low energy, especially during the first few weeks, as the body adapts to lower blood pressure levels.
5. Headaches
These can occur during dose changes or as vessels adjust, but they often fade over time.

6. Awareness of Heartbeat (Palpitations)
You might notice a gentle thumping in your chest or neck, even if your heart rate isn’t fast. This stems from increased blood flow.
7. Leg Heaviness or Warmth
Your legs may feel heavier during activity, like after a short walk, due to enhanced circulation in the limbs.
Here’s a quick comparison table to help visualize these:
| Side Effect | Possible Reason | When It Often Occurs |
|---|---|---|
| Swelling in ankles/feet | Fluid shifts from vessel widening | Later in the day, after sitting/standing |
| Facial flushing | Increased blood flow to skin | Brief episodes, possibly after meals |
| Dizziness | Blood pressure drop | When standing up quickly |
| Fatigue | Body adjusting to lower pressure | Irregular, often early on |
| Headache | Vessel changes | Temporary during adjustments |
| Heartbeat awareness | Enhanced circulation | At rest or lying down |
| Leg heaviness | More blood flow to limbs | During or after activity |
Simple Habits to Help Manage These Sensations
While these steps aren’t a replacement for medical advice, many people find they support comfort during treatment. Research and patient guidance suggest focusing on circulation and daily routines.
- Stay active with gentle movement: Short walks or light stretching several times a day can promote better blood flow and reduce fluid buildup.
- Drink plenty of water: Proper hydration helps maintain stable blood flow—aim for consistent intake throughout the day.
- Elevate your legs when resting: Prop them up for 15-20 minutes after long sitting periods to encourage fluid drainage.
- Avoid sudden position changes: Rise slowly from sitting or lying to minimize dizziness.
- Track your symptoms: Note when they appear and any patterns (like after meals or activity) to discuss with your provider.
- Wear comfortable compression socks: These can help with leg swelling for some people.
- Limit salt intake: Reducing sodium may ease fluid retention.
Here’s a practical daily checklist:
- Walk gently 2-3 times per day (start slow).
- Sip water regularly—keep a bottle handy.
- Elevate legs as needed in the evening.
- Stand up gradually.
- Log symptoms in a simple journal.
Real-Life Examples from Others
Many people share similar experiences. One person noticed ankle swelling after long workdays but felt better after adding short walks and leg elevation. Another tracked flushing episodes and realized they linked to certain meals, which helped reduce worry. These stories show how awareness and small adjustments can make a difference.
When to Talk to Your Healthcare Provider
If any sensation feels concerning, persists, or worsens, reach out to your doctor. They can adjust your dose or explore other options. Regular check-ins ensure your treatment stays safe and effective.

FAQ
How long do amlodipine side effects usually last?
Most mild effects improve within a few weeks as your body adjusts, though some may persist longer. Always consult your provider if they bother you.
Can lifestyle changes make side effects go away completely?
They may help reduce how noticeable they are, but effects vary by person. Your doctor can offer personalized tips.
Is it common to have no side effects at all?
Yes—many people take amlodipine without noticeable issues, especially at lower doses.
This article is for informational purposes only and does not replace professional medical advice. Always consult your healthcare provider for personalized guidance regarding your medications and health.
(Word count: 1,248)