Many women go about their daily lives without noticing subtle shifts in their bodies until something feels off. These small changes can sometimes point to broader health concerns, leaving you feeling anxious and uncertain about what to do next. But understanding these signals early on empowers you to take proactive steps toward your well-being. In this article, we’ll explore four key changes that research highlights as important to watch for, and I’ll share a surprising insight at the end that could change how you approach your routine check-ups.

Understanding Why Early Awareness Matters
Breast health is a vital part of overall wellness for women, and staying informed can make a significant difference. According to organizations like the Mayo Clinic, many changes in the breast area are benign, but some warrant attention from a healthcare professional. Regular self-exams and screenings help in noticing these shifts sooner.
But that’s not all. Studies from the American Cancer Society show that awareness of your body’s normal state is key. When you know what feels typical, you’re better equipped to spot deviations. This isn’t about fear—it’s about empowerment through knowledge.
The Role of Routine Self-Exams
One actionable step you can take right away is incorporating monthly self-exams into your routine. Here’s how to do it step by step:
- Stand in front of a mirror with your arms at your sides. Look for any visible changes in size, shape, or skin texture.
- Raise your arms overhead and check again for the same.
- Lie down, using the pads of your fingers to feel your breasts in a circular motion, covering the entire area from collarbone to abdomen.
- Repeat while standing or in the shower, where skin is slippery and easier to examine.
- Note any differences and report them to your doctor if they persist.
This simple habit, recommended by breast health experts, takes just a few minutes and can become second nature.
Sign 1: Noticing Unusual Lumps or Thickening
A common change many women encounter is the development of a lump or area of thickening in the breast or underarm. This might feel different from the surrounding tissue—perhaps firmer or uneven. Research from the Centers for Disease Control and Prevention (CDC) indicates that while most lumps are non-cancerous, like cysts or fibroadenomas, they should never be ignored.
Here’s the interesting part: These lumps can sometimes appear gradually, giving your body time to signal something’s amiss. If it’s painless and doesn’t change with your menstrual cycle, that’s a cue to consult a professional.
To check effectively, use the self-exam technique mentioned earlier. If you find something new, track it for a cycle or two, but don’t delay seeking advice if it concerns you.
When to Seek Professional Guidance
Not every lump requires immediate action, but persistence is key. The Breast Cancer Research Foundation suggests scheduling an appointment if the lump remains after your period or grows. Early conversations with your doctor can provide peace of mind through ultrasounds or mammograms.

Sign 2: Changes in Breast Size or Shape
Have you ever noticed one breast looking slightly different from the other? Subtle alterations in size, shape, or contour can occur over time. According to Mayo Clinic experts, these changes might stem from hormonal fluctuations, but they can also signal underlying issues.
Sustainability in monitoring is crucial here. A study published in the Journal of the National Cancer Institute notes that gradual shifts, unlike sudden ones from injury, deserve attention. This could manifest as asymmetry that wasn’t there before.
But wait, there’s more to consider. Pregnancy, weight changes, or aging can play roles, so context matters. Still, if the difference feels unexplained, it’s worth noting.
Practical Tips for Monitoring
Keep a journal of your observations. Every month, after your period, take photos or notes on appearance. This visual record, as advised by health educators, helps track patterns and discuss them accurately with your healthcare provider.
| Common Causes of Size Changes | When to Worry |
|---|---|
| Hormonal cycles | Persistent asymmetry without explanation |
| Weight gain/loss | Sudden, one-sided swelling |
| Aging or menopause | Accompanied by other signs like pain |
This table breaks down everyday factors versus potential red flags, making it easier to assess.
Sign 3: Skin Changes Like Dimpling or Redness
Skin on the breast can tell a story too. Dimpling, where the skin pulls in like an orange peel, or unexplained redness might appear. The CDC lists these as notable because they can indicate inflammation or blockages beneath the surface.
Truth be told, these aren’t always dramatic—they might start mildly and progress. A report from Breastcancer.org explains that such textures result from tissue pulling, often subtle at first.
Don’t overlook flaking or scaling around the nipple area either. While dry skin is common, persistent issues differ.
Steps to Address Skin Concerns
Gently moisturize the area daily with fragrance-free lotion to rule out dryness. If changes linger beyond a week, capture a photo and share it with your doctor. They might recommend a dermatological check or imaging.
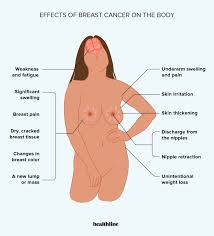
Sign 4: Nipple Changes Including Discharge or Inversion
Nipples can undergo transformations that are easy to miss if you’re not attentive. Inversion, where the nipple turns inward, or unexpected discharge (clear, bloody, or otherwise) are highlighted by the American Cancer Society as important observations.
Here’s a key insight: These might not hurt, which is why they’re often dismissed. But research shows they can precede other symptoms by months.
Pain in the nipple or surrounding area, though less common early on, shouldn’t be ignored if it’s new.
How to Respond Effectively
Inspect your nipples during self-exams for any retraction or fluid. If discharge occurs, note the color and amount. Avoid squeezing, as it can irritate. Instead, seek a professional evaluation promptly.
- Clear or milky discharge: Often hormonal, but check if pregnant or breastfeeding.
- Bloody or colored: More concerning; see a doctor soon.
- Inversion: If sudden and not lifelong, investigate.
This bullet list simplifies what to watch, based on expert guidelines.
Additional Factors Influencing Breast Health
Beyond these signs, lifestyle plays a role. Maintaining a healthy weight, limiting alcohol, and exercising regularly, as per CDC recommendations, support overall breast wellness.
Genetic factors matter too. If family history includes breast concerns, discuss screening options like genetic testing with your doctor.
And remember, age isn’t a barrier—changes can happen at any stage, though risk increases after 40.
The Importance of Professional Screenings
Routine mammograms, starting at age 40 or earlier if high-risk, complement self-awareness. The U.S. Preventive Services Task Force advises biennial screenings, which detect changes invisible to touch.
Combining this with annual clinical exams creates a robust defense.
Wrapping It Up: Empowering Your Health Journey
Recognizing early breast changes—like lumps, size shifts, skin alterations, or nipple issues—fosters proactive health management. By staying vigilant and incorporating self-exams, you’re taking meaningful steps. And that surprising insight I promised? Many women discover that consistent tracking not only spots issues early but also reduces anxiety through familiarity with their bodies.
Frequently Asked Questions
What should I do if I notice a change but it’s not painful?
Even painless changes deserve attention. Schedule a visit with your healthcare provider for evaluation, as pain isn’t always present in early stages.
How often should I perform a breast self-exam?
Experts recommend monthly, ideally a few days after your period ends when breasts are least tender. Consistency helps you notice patterns.
Are there lifestyle changes that support breast health?
Yes, maintaining a balanced diet, regular exercise, and avoiding smoking can contribute positively, according to health studies.
Remember, this information is for educational purposes only and not a substitute for professional medical advice. Always consult a qualified healthcare provider for any health concerns or before making changes to your health routine.






