Pancreatic issues often develop quietly without obvious signals, leaving many people feeling off but unsure why. These vague shifts in how your body feels can build gradually, making them easy to brush off as normal fatigue or minor digestive upset. Yet paying closer attention to these changes can prompt timely conversations with your doctor. And toward the end of this guide, we’ll uncover one lesser-known clue that ties several of these shifts together in a surprising way.
Why Early Awareness Matters for Pancreatic Health
The pancreas plays a key role in digestion and blood sugar regulation, but problems here rarely announce themselves loudly at first. Research from organizations like the American Cancer Society shows that many pancreatic conditions produce no clear symptoms early on, allowing them to progress unnoticed.
By the time more noticeable changes appear, the underlying issue may have advanced. That’s why recognizing subtle patterns now can make a real difference in getting checked sooner rather than later.
But that’s not all—understanding how these body signals connect can help you advocate for yourself more effectively.
Common Body Changes to Watch For
Here are some of the most frequently reported shifts that studies link to pancreatic concerns. Keep in mind, these can stem from many other causes too, but persistence warrants attention.
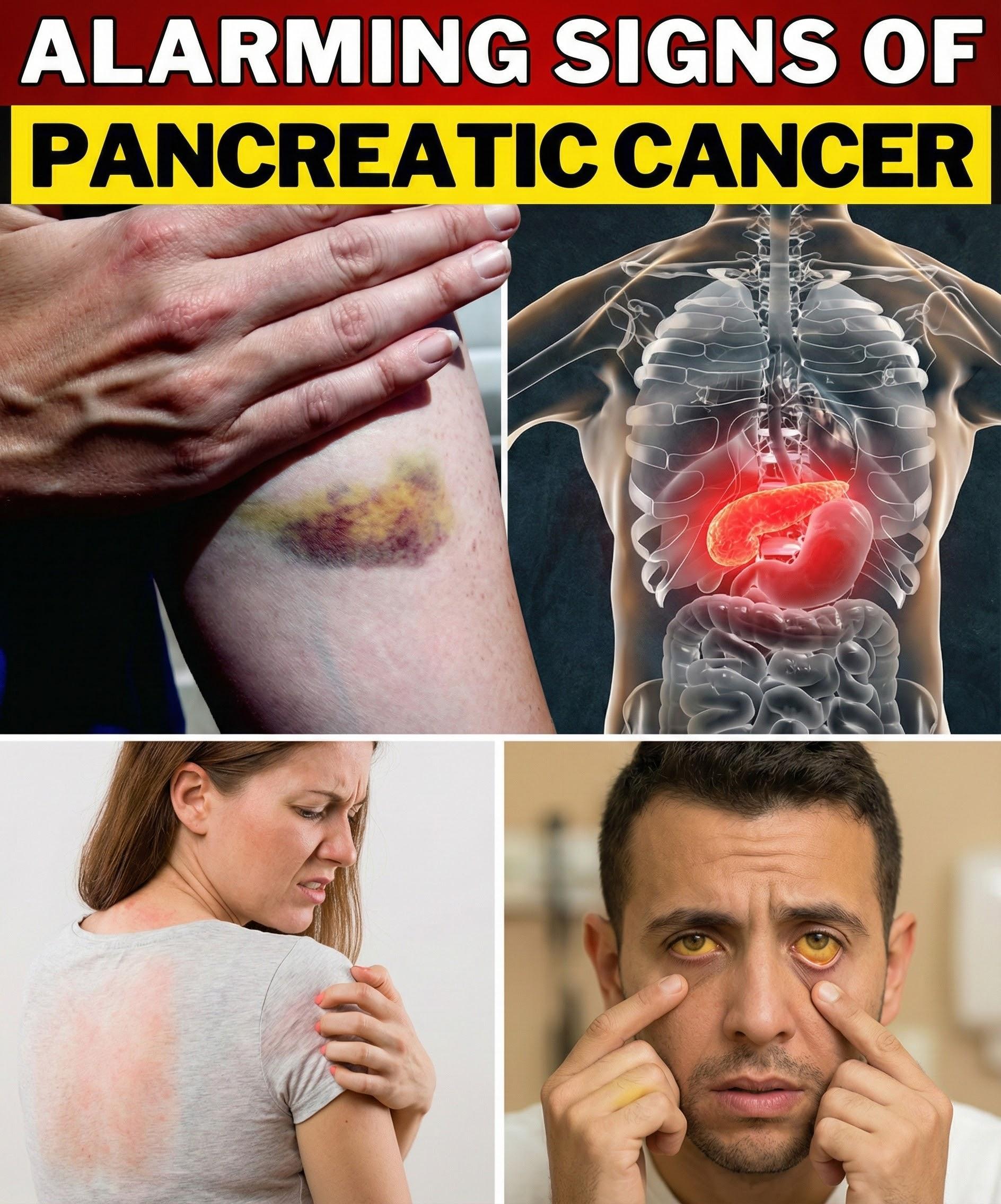
Yellowing of the Skin or Eyes (Jaundice)
One noticeable change is a yellowish tint to the skin or the whites of the eyes. This happens when bilirubin builds up due to blocked bile flow.
It often comes with darker urine or lighter stools. According to Mayo Clinic resources, this can appear gradually and is one of the more specific signals.
Persistent Itchy Skin
Many people describe an unexplained itch that worsens over time, sometimes all over but especially on the palms or soles.
This discomfort can disrupt sleep and daily life. Sources like the Pancreatic Cancer Action Network note it’s tied to the same bile buildup as jaundice.
The really frustrating part? Over-the-counter remedies often provide little relief.

Unexplained Weight Loss
Losing weight without trying—especially if appetite drops or food doesn’t appeal as much—can feel confusing.
Digestion may not work as efficiently, leading to fewer nutrients absorbed. Studies referenced by WebMD highlight this as a common early shift.
Upper Abdominal or Back Pain
A dull ache in the upper abdomen that sometimes radiates to the back is another frequent report.
It might worsen after eating or when lying down. The American Cancer Society explains this can result from pressure on nearby structures.
Here’s the interesting twist: the pain often feels vague at first, coming and going rather than constant.
Digestive Changes
Shifts like floating, greasy stools, nausea after meals, or new bloating can signal digestion issues.
These occur because pancreatic enzymes aren’t reaching the intestines properly.
- Greasy or foul-smelling stools
- Increased gas or indigestion
- Feeling full quickly
Research shows these changes often overlap with common gut problems, leading to delays in further checks.
New-Onset Diabetes or Blood Sugar Changes
Suddenly developing diabetes, especially after age 50, or seeing existing diabetes become harder to control can be a red flag.
The pancreas regulates insulin, so disruptions here affect blood sugar. Healthline reviews indicate this as a potential early indicator.
Fatigue and Weakness
Feeling unusually tired despite rest is common, often tied to the body’s extra effort managing inflammation or poor nutrient absorption.
This isn’t your typical tiredness—it lingers and impacts daily activities.
Less Common But Important Signals
Some changes appear in fewer cases but still deserve mention:
- Swelling or tenderness in a limb (possibly linked to clotting tendencies)
- Loss of appetite leading to further weight drop
The truth is, no single change confirms anything on its own. It’s the combination and persistence that matters most.
Practical Steps to Take If You Notice These Changes
Don’t wait for things to worsen—here’s a simple approach:
- Track your symptoms for a week or two, noting when they occur and severity.
- Schedule a doctor’s visit and share your notes clearly.
- Mention any family history or risk factors like smoking.
- Ask about basic tests like blood work or ultrasound if symptoms persist.
Acting promptly gives the best chance for clear answers.
Comparing Common Causes of Similar Changes
To help put things in perspective:
| Change | Often Seen In | Key Difference with Pancreatic Concerns |
|---|---|---|
| Jaundice | Gallstones, liver issues | Painless, gradual onset |
| Itchy Skin | Allergies, dry skin | Widespread, no rash |
| Weight Loss | Diet changes, stress | Unintentional, with digestive shifts |
| Abdominal Pain | Indigestion, ulcers | Radiates to back, persistent |
This isn’t diagnostic—just a way to think through patterns.
Final Thoughts
Your body communicates in subtle ways, and tuning in can lead to earlier clarity on health concerns. While most of these changes have benign explanations, ignoring persistent ones isn’t worth the risk.
And here’s that lesser-known connection we hinted at earlier: sometimes, migratory superficial vein inflammation (known as Trousseau’s sign) appears alongside other shifts, serving as a rare but notable clue in some pancreatic cases.
Stay proactive—your awareness today could shape better outcomes tomorrow.
Frequently Asked Questions
How soon should I see a doctor for these changes?
If any persist for more than two weeks or worsen, make an appointment right away. Early discussions are always better.
Are these changes always serious?
No—many resolve on their own or stem from minor issues. But combinations, especially with weight loss or jaundice, need evaluation.
Can lifestyle factors influence pancreatic health?
Yes, maintaining a healthy weight, limiting alcohol, and avoiding smoking support overall wellness, per general health guidelines.
Disclaimer: This information is for educational purposes only and not a substitute for professional medical advice. Always consult a qualified healthcare provider for personal concerns, as only they can provide proper evaluation and guidance.






