Many people take everyday medications to manage conditions like pain, heartburn, high blood pressure, or infections. These drugs can be helpful, but some may influence kidney function, especially with long-term use or in certain situations. Research shows that certain medications are linked to a higher chance of kidney issues in some individuals. Understanding these potential effects can help you have informed conversations with your doctor.
The good news? Awareness and regular check-ups can make a big difference. In this article, we’ll explore 10 common types of medications that studies have associated with kidney concerns. We’ll look at what the evidence says and share practical steps you can take. By the end, you’ll have a clearer picture of how to support your kidney health while managing your conditions.
Why Kidney Health Matters as We Age
Over time, kidneys naturally filter less efficiently, and factors like dehydration, high blood pressure, or diabetes can add stress. Medications play a role too—some by reducing blood flow to the kidneys or affecting tubular cells.
Studies from sources like the National Kidney Foundation and Mayo Clinic note that drug-related factors contribute to a portion of kidney issues. But not everyone experiences problems, and risks often depend on dose, duration, and individual health.
That’s why monitoring is key. Let’s dive into the medications most often discussed in research.
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs like ibuprofen and naproxen are go-to options for pain and inflammation.
Research indicates that prolonged or high-dose use can reduce blood flow to the kidneys, especially if you’re dehydrated or have existing risks. Studies, including those reviewed by the National Kidney Foundation, link chronic NSAID use to a higher chance of kidney concerns.
Tip: Use the lowest effective dose for the shortest time. Talk to your doctor about alternatives like acetaminophen for ongoing needs.
2. Proton Pump Inhibitors (PPIs)
PPIs such as omeprazole help with acid reflux and heartburn.
Long-term use has been associated in observational studies, like one in JAMA Internal Medicine, with a potential increased risk of chronic kidney issues. The exact reason isn’t fully clear, but monitoring is recommended for extended use.
Many people feel relief knowing shorter courses or lifestyle changes can sometimes reduce reliance on them.
3. Certain Antibiotics (e.g., Aminoglycosides)
Antibiotics like gentamicin treat serious infections.
These can affect kidney tubules, as noted in StatPearls and other reviews. Risk is higher with prolonged courses or in hospital settings.
Doctors often monitor levels closely and choose alternatives when possible.

4. ACE Inhibitors and ARBs
Medications like lisinopril or losartan manage blood pressure and often protect kidneys in conditions like diabetes.
They can sometimes cause a temporary rise in creatinine, but studies show they generally slow kidney decline in many cases. Close monitoring helps adjust as needed.
5. Diuretics
“Water pills” like furosemide help with swelling and blood pressure.
They can lead to dehydration if not balanced with fluids, potentially stressing kidneys. Research emphasizes using them carefully in those with reduced kidney function.
Staying hydrated and regular checks can help.
6. Statins
Statins lower cholesterol and reduce heart risks.
Most evidence shows benefits, even in kidney disease, but rare cases link high doses to muscle issues that indirectly affect kidneys.
Overall, guidelines support their use for cardiovascular protection.
7. Lithium
Used for mood stabilization.
Long-term use can impact kidney concentrating ability or function, as discussed in reviews. Regular blood tests are standard to catch changes early.
Comparison of Common Medications and Kidney Considerations
| Medication Class | Common Examples | Key Research Notes | Monitoring Suggestions |
|---|---|---|---|
| NSAIDs | Ibuprofen, Naproxen | Linked to reduced kidney blood flow in some studies | Urine tests, creatinine checks |
| PPIs | Omeprazole, Esomeprazole | Observational links to higher CKD risk | Periodic kidney function labs |
| Aminoglycosides | Gentamicin | Tubular effects in prolonged use | Dose monitoring, shorter courses |
| ACE Inhibitors/ARBs | Lisinopril, Losartan | Often protective; monitor for changes | Regular eGFR and potassium |
| Diuretics | Furosemide | Risk with dehydration | Fluid balance, electrolyte checks |
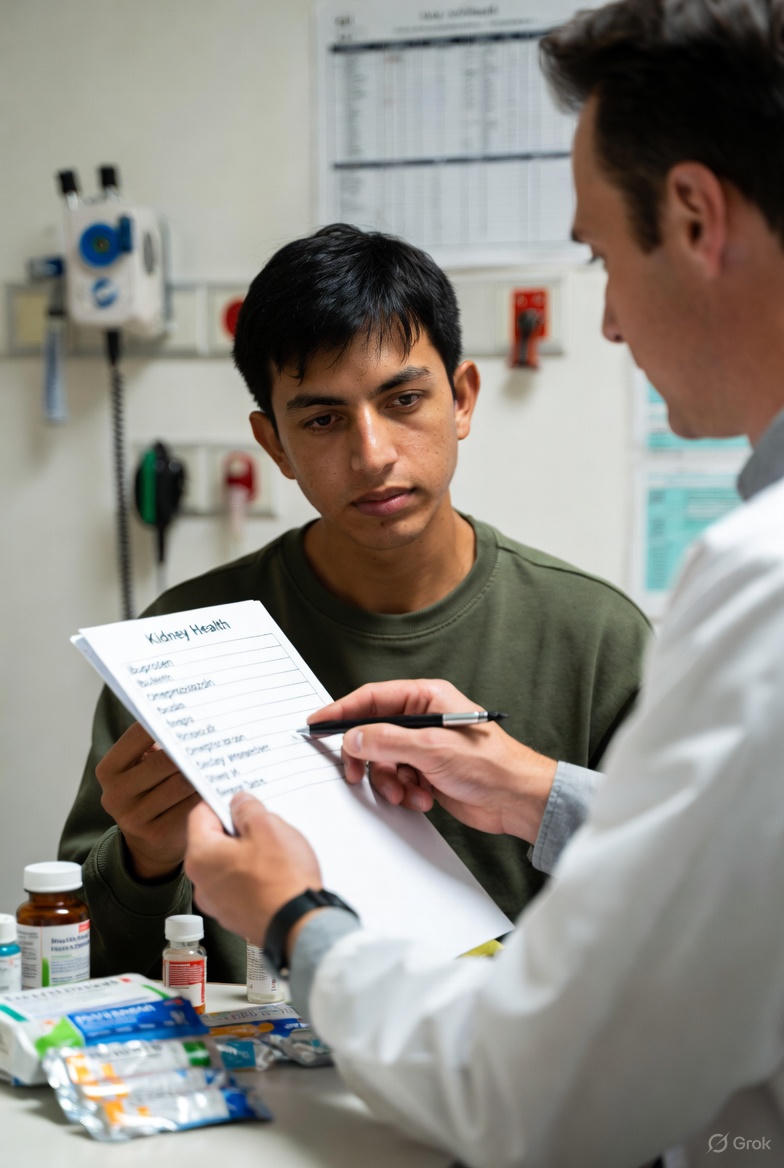
Practical Steps to Support Your Kidney Health
Here are actionable tips based on expert recommendations:
- Stay hydrated—aim for consistent water intake daily.
- Get regular check-ups, including blood and urine tests for creatinine and protein.
- Review your medications with your doctor or pharmacist annually.
- Discuss any new symptoms like swelling or fatigue promptly.
- Consider lifestyle supports: balanced diet, moderate exercise, and blood pressure control.
These small habits can add up to meaningful protection.
Other Medications to Discuss with Your Doctor
- Certain antivirals or chemotherapy agents: Used in specific conditions, with known kidney monitoring protocols.
- Immunosuppressants: Important for transplants or autoimmune issues, but require close oversight.
Every situation is unique—your healthcare team can tailor advice.
Frequently Asked Questions
1. How often should I check my kidney function if taking these medications?
Guidelines suggest at least yearly for many, or more frequently if risks are higher. Ask your doctor for a personalized plan.
2. Can I stop a medication if I’m worried about my kidneys?
Never stop without guidance—sudden changes can affect your condition. Discuss options like dose adjustments or alternatives.
3. Are there signs of kidney changes I should watch for?
Symptoms like persistent fatigue, swelling, or changes in urination warrant a prompt check-in with your provider.
This information is for educational purposes only and is not a substitute for professional medical advice. Always consult your healthcare provider about your medications and any concerns regarding kidney health. Regular monitoring and open discussions are the best ways to stay informed and proactive.